Hidden Varicose Veins

Understanding a Common but Overlooked Vein Problem
Varicose veins and their hidden counterparts affect many worldwide, yet many remain unaware of the condition until symptoms become hard to ignore.
Hidden varicose veins lie deeper beneath the skin. They can cause pain, heaviness, and swelling even when no visible veins are present.
At the forefront of advanced vein care in Dubai, Dr. Ashok Gupta brings over 30 years of expertise in vascular surgery, specializing in minimally invasive treatments such as LASER and RFA (Radiofrequency Ablation).
Known for his compassionate, evidence-based approach, Dr. Gupta focuses on restoring healthy circulation and helping patients lead active, pain-free lives through precise diagnosis and personalized care.
What are “hidden” varicose veins?
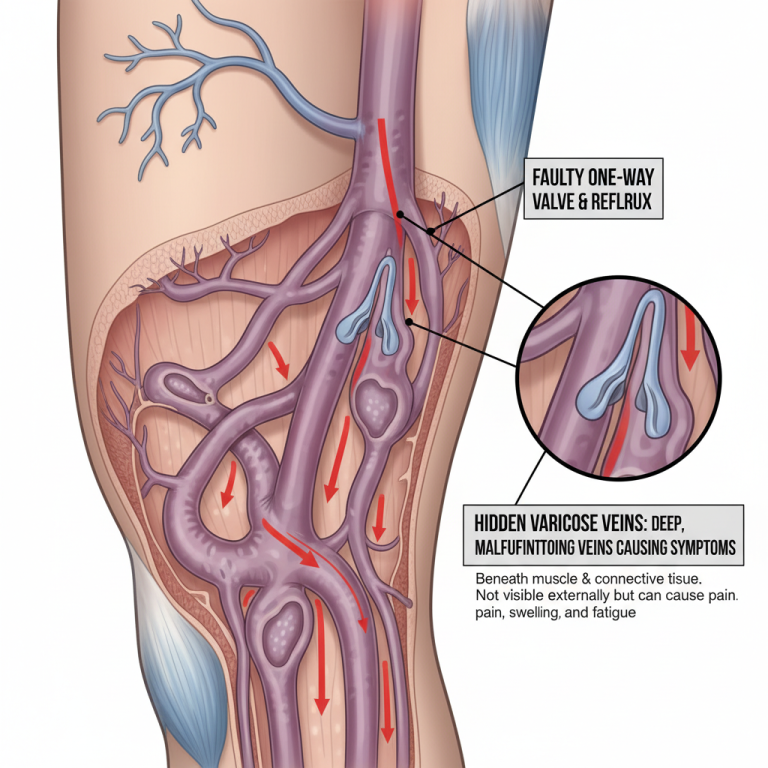
Hidden varicose veins are more profound, malfunctioning leg veins with the same underlying problem as visible ones. The main culprits are faulty one-way valves and weakening vein walls that let blood fall back with gravity (venous reflux), pool, and raise pressure in the tissues. Because they lie beneath muscle or connective tissue, they are not apparent on inspection but can be just as symptomatic.
Hidden varicose veins symptoms
The early stage varicose veins symptoms include the following:
- Dull ache or throbbing after sitting or standing
- Ankle and calf swelling that worsens in the evening
- Leg heaviness or easy fatigue
- Night cramps or “restless legs” sensations
- Itching, discoloration, or skin thickening around the ankle
These symptoms warrant a venous evaluation even if your legs look “normal.”
The science has shifted: varicose veins progress upwards, not down.
Classic teaching blamed pressure from above. The earliest valve failures usually start low in the leg and then progress upwards (“ascending” pattern).
When a lower valve fails, it disturbs flow and reduces the beneficial shear across the next valve; that reduced flow can “switch off” the valve-maintainenance, leading the next valve to fail. This reframes both diagnosis and treatment priorities.
If only upper-thigh reflux is treated without addressing lower-leg sources, recurrence is more likely. Mapping all reflux pathways (especially low in the leg) and ablating the diseased segments restores normal hemodynamics and protects the remaining valves.
How do we find hidden disease?
Because you cannot rely on the eye, the proper test is key:
- Duplex/Doppler ultrasound is painless and noninvasive: It shows the direction and speed of flow, localizes refluxing segments, and confirms which veins need treatment.
- Venography: Contrast X-ray for select complex cases.
Diagnosis relies on duplex/Doppler ultrasound, and treatments like RFA, EVLA, foam (e.g., Varithena), and ultrasound-guided sclerotherapy close the faulty veins and restore healthy flow.
Deep varicose veins treatment
All aim to close refluxing pathways so blood reroutes through healthy veins:
- Radiofrequency ablation (RFA)
- Endovenous laser ablation (EVLA/EVLT)
- Foam therapy (e.g., Varithena) for non-straight, tortuous, or deeper tributaries
- Ultrasound-guided sclerotherapy for residual branches/tributaries
- These are clinic-based, require only local anesthesia in most cases, and typically involve rapid return to activity with compression and walking.
When to seek care
- Persistent ache, heaviness, evening swelling, or night cramps
- Itching/discoloration near the ankle
- A history of “failed” vein procedures or rapid recurrence
- Skin changes, eczema, healed or active ankle ulcers
- Early intervention reduces the risk of chronic venous insufficiency, clots, bleeding, and ulceration.
- Varicose vein cancer symptoms are unrelated, but a doctor should check for swelling or skin changes.
- Bulging veins in legs, not varicose, may occur after exercise or heat exposure and are usually harmless unless painful.
Dr. Ashok Gupta: Guideline-based vein care in Dubai
With expertise spanning over three decades focused on lower-limb venous disease and circulation, Dr. Gupta offers:
Minimally invasive expertise
Laser and RFA, ultrasound-guided treatments, and sclerotherapy tailored to your needs.
Whole-leg mapping
Diagnosis anchored in duplex ultrasound with attention to lower-leg sources of reflux (per the ascending-failure model).
Stepwise therapy & follow-up
Lifestyle support, compression, targeted ablation and branch work, with long-term surveillance to prevent recurrence.
Comprehensive service
Varicose/spider veins, DVT, lymphedema, diabetic foot care. You will get an honest, evidence-based plan that treats the cause, not just the appearance, and helps you return to an active, comfortable life.
Ready to stop guessing and start treating the cause?
Take the first step toward healthier legs today.
Book your consultation with Dr. Ashok Gupta, and discover the most effective way to diagnose and treat hidden varicose veins before they lead to visible problems.
FAQs
How do you treat hidden varicose veins?
Hidden varicose veins are treated with minimally invasive methods, such as laser (EVLA), radiofrequency ablation (RFA), foam therapy (Varithena), or ultrasound-guided sclerotherapy, to close faulty veins and restore healthy blood flow.
When should I worry about varicose veins?
Seek medical care if you have pain, swelling, skin discoloration, itching, or ulcers, even without visible bulging veins, as these may indicate deeper venous disease.
When to worry about varicose veins in pregnancy?
If varicose veins cause severe pain, redness, or swelling during pregnancy, consult a doctor. Most pregnancy-related veins improve after delivery, but should still be monitored.
How to treat varicose veins in kids?
Pediatric varicose veins are rare and usually need a vascular specialist’s evaluation to rule out congenital or circulatory issues. Treatment depends on the cause and severity.
Can varicose veins cause shin pain?
Yes, faulty veins can cause pressure buildup in the lower legs, leading to shin pain, heaviness, or throbbing, especially after standing long hours.
How to get rid of varicose veins naturally in 3 minutes?
There is no quick, natural cure. However, leg elevation, light movement, and cold compresses can provide short-term relief. Long-term control requires proper medical treatment and lifestyle care
